That knot in your chest when you realize you’ll be home alone tonight. The racing thoughts. The desperate urge to call someone—anyone—just to hear another voice. If this sounds painfully familiar, you’re experiencing something very real, and you’re not overreacting.
Fear of being alone, also called autophobia or monophobia, is an anxiety disorder that affects more people than you might think. It’s not about enjoying company or preferring to be around others. It’s about the overwhelming panic that grips you when faced with solitude, even in your own home where you should feel safest.
Here’s something that might surprise you: You don’t have to actually be alone to experience this fear. Many people with autophobia feel intense anxiety even in crowds, worrying about people leaving or having to eventually go home by themselves.
If you’re reading this because you’re struggling, take a breath. What you’re experiencing has a name, it’s treatable, and there are concrete steps you can take—starting today—to feel better.
What Is Autophobia? Understanding the Fear of Being Alone
Autophobia is a specific phobia characterized by intense, persistent fear of being alone or isolated. Unlike ordinary loneliness—which everyone experiences when lacking meaningful social connections—autophobia triggers genuine terror at the thought or reality of solitude.
The name comes from the Greek words “auto” (self) and “phobia” (fear). You might also hear it called:
- Monophobia (fear of being alone)
- Isolophobia (fear of isolation)
- Eremophobia (fear of solitude)
While autophobia isn’t listed as a separate disorder in the DSM-5 (the manual mental health professionals use for diagnosis), it falls under the category of “specific phobias”—situational type. This means it’s classified and diagnosed as code 300.29 (F40.248) in the DSM-5 and code 6B03 in the ICD-11.[^1]
The Numbers: You’re Far From Alone
If you’re dealing with autophobia, here’s something you need to know: millions of people share your experience.
An estimated 9.1% of U.S. adults experience a specific phobia in any given year, which translates to approximately 19 million Americans.[^2] Over their lifetime, up to 12.5% of the U.S. population will experience a specific phobia—that’s more than 1 in 8 people.[^3]
The global picture is similar. Cross-national research spanning 22 countries found that 7.4% of people worldwide experience specific phobias in their lifetime, with current (12-month) prevalence at 5.5%.[^4] Recent studies indicate that over a quarter of the whole population is at risk of developing some form of specific phobia throughout their lives.[^5]
Gender differences are significant: Past year prevalence of specific phobia among adults is higher for females (12.2%) than for males (5.8%).[^2] This 2:1 ratio appears consistently across cultures and age groups.
And here’s what matters most: Of adults with specific phobia in the past year, 48.1% had mild impairment, 30% had moderate impairment, and 21.9% had serious impairment.[^2] This means that while autophobia can be challenging, nearly half of people with specific phobias experience only mild effects—and treatment can significantly reduce symptoms for everyone.
Autophobia vs. Loneliness: What’s the Difference?
This is crucial to understand: autophobia and loneliness are not the same thing.
Loneliness is:
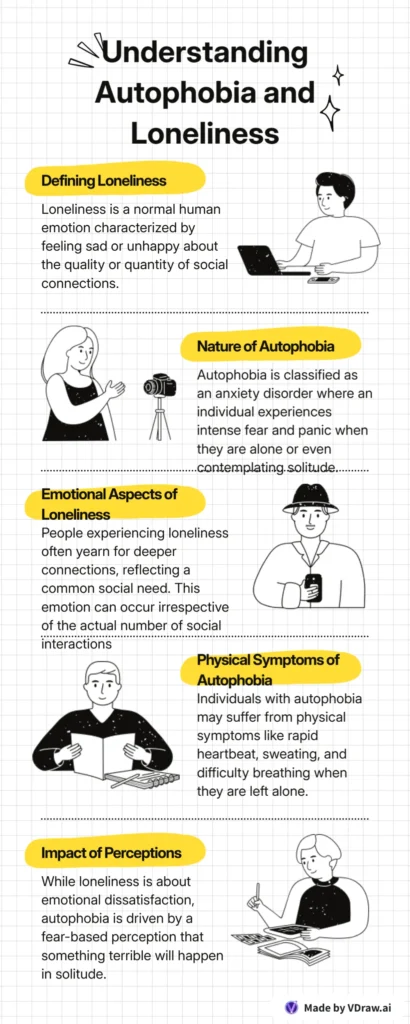
- A normal human emotion
- Feeling sad or unhappy about the quality or quantity of your social connections
- Wishing you had more meaningful relationships
- Generally not causing physical panic symptoms
Autophobia is:
- An anxiety disorder
- Experiencing intense fear and panic when alone or thinking about being alone
- Feeling terrified even when you have many loved ones in your life
- Causing physical symptoms like rapid heartbeat, sweating, and difficulty breathing
- Believing something bad will happen when you’re by yourself
With autophobia, you can be surrounded by friends and family and still feel the fear—because it’s not really about whether you have social connections. It’s about the anticipation of being separated from others and the anxiety that brings.
For more on how autophobia differs from other isolation-related fears, read about agoraphobia, which involves fear of being in places where escape might be difficult.
Recognizing the Symptoms: Physical, Emotional & Behavioral Signs
Autophobia affects everyone differently, but most people experience a combination of physical, emotional, and behavioral symptoms. These symptoms typically arise when you’re alone, when you anticipate being alone, or even when you feel excluded in a group.
Physical Symptoms
Your body responds to the fear of being alone as if you’re facing a real threat:
- Heart palpitations or racing heartbeat
- Shortness of breath or feeling like you can’t get enough air
- Excessive sweating or cold sweats
- Trembling or shaking
- Dizziness or lightheadedness
- Nausea or upset stomach
- Chest tightness or pain
- Hot or cold flashes
- Difficulty swallowing
- Headaches
These are classic panic attack symptoms, and they’re your body’s fight-or-flight response kicking in when there’s no actual danger present. If you experience similar symptoms in specific situations, like fear of being without your phone, you might also relate to nomophobia.
Emotional & Psychological Symptoms
The mental burden of autophobia can be just as intense:
- Overwhelming dread about being left alone
- Persistent worry about people leaving you
- Fear of abandonment, even by close friends and family
- Feeling unsafe unless someone else is nearby
- Believing something terrible will happen when you’re alone (medical emergency, intruder, disaster)
- Feeling unwanted or unloved
- Racing thoughts that won’t stop
- Feeling detached from yourself or your surroundings (depersonalization)
- Constant need for reassurance from others
- Fear of dying alone or being unable to get help
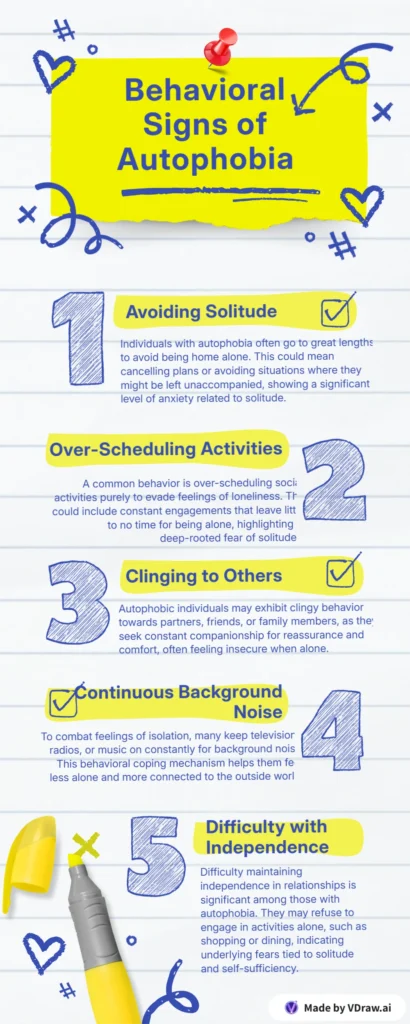
Behavioral Symptoms
Autophobia changes how you live your daily life:
- Avoiding being home alone at all costs
- Over-scheduling social activities just to avoid solitude
- Clinging to partners, friends, or family members
- Keeping TV, radio, or music on constantly for background noise
- Making unnecessary phone calls just to hear another voice
- Sleeping with lights on or unable to sleep when alone
- Following people around (even partners to different rooms)
- Refusing to do activities alone (shopping, errands, meals)
- Difficulty maintaining independence in relationships
- Staying in unhealthy relationships out of fear of being alone
Duration matters: For a diagnosis of autophobia, these symptoms must persist for at least six months and significantly interfere with your daily functioning, relationships, or work.[^1]
What Causes Autophobia? The Roots of Fear
The exact causes of autophobia aren’t fully understood, but research points to several key factors. For most people, it’s a combination of multiple triggers rather than one single cause.
Childhood Trauma & Abandonment
Early experiences shape how we perceive safety and attachment. Common childhood triggers include:
- Parental divorce or separation during formative years
- Death of a parent or primary caregiver
- Neglect or inconsistent caregiving (being left alone frequently as a child)
- Being lost or separated from parents in public places
- Witnessing or experiencing abandonment (physical, emotional, or financial)
- Unstable home environment with caregivers who were unreliable
Research shows that ambivalently attached children who experienced unreliable caregivers were constantly afraid of being alone and in danger, with this fear of separation or abandonment continuing throughout childhood and adulthood.[^6] These experiences can create deep-seated beliefs that being alone equals danger or that people you depend on will inevitably leave.
Attachment Style: The Foundation of Fear
Attachment theory provides one of the strongest explanations for why autophobia develops. Your attachment style—formed in early childhood and carried into adulthood—significantly influences your response to being alone.
Anxious-preoccupied individuals often experience anxiety and insecurity in relationships, leading to dependency and fear of abandonment.[^7] The anxiety dimension assesses the degree to which individuals worry about being underappreciated or abandoned by their romantic partners, with highly anxious individuals heavily invested in their relationships and yearning to get closer emotionally to feel more secure.[^8]
Recent research found that fear of abandonment was positively correlated with both attachment insecurity (r = .62, p < .001) and psychosomatic symptoms (r = .51, p < .001),[^9] demonstrating the powerful link between attachment fears and physical anxiety symptoms.
The three primary attachment styles associated with autophobia:
Anxious-Preoccupied Attachment:
- Constant worry about others leaving
- Need for frequent reassurance
- Difficulty trusting that people will stay
- Fear of being left vulnerable and alone, leading to chronic vigilance that may continue throughout life and contribute to anxiety disorders[^6]
Fearful-Avoidant Attachment:
- Desire for closeness combined with fear of rejection
- Conflicted feelings about relationships
- Avoiding intimacy to protect from potential abandonment
Dependent Attachment Patterns:
- Feeling incapable of functioning independently
- Excessive reliance on others for decision-making
- Low self-confidence when alone
Traumatic Events While Alone
Sometimes a single frightening experience while alone can trigger autophobia:
- Home invasion or burglary when you were by yourself
- Medical emergency with no one to help
- Panic attack while alone, creating fear of future attacks
- Witnessing violence or a traumatic event without support
- Being mugged or attacked while alone
- Severe illness or injury when isolated
These experiences create a mental association: alone = vulnerable to danger.
Mental Health Conditions
Autophobia frequently co-occurs with other mental health disorders:
- Panic Disorder: Fear of having a panic attack with no one to help
- Borderline Personality Disorder (BPD): Intense fear of rejection and abandonment
- Dependent Personality Disorder (DPD): Feeling incapable of self-care
- Generalized Anxiety Disorder: Overall high anxiety levels
- Agoraphobia: Fear of being in places where help might not be available
- Post-Traumatic Stress Disorder (PTSD): Trauma-related fear responses
- Social Anxiety: Fear of isolation or being excluded from groups
- Depression: Low self-worth and fear of being unwanted
Life Transitions & Modern Triggers
Recent life changes can trigger or worsen autophobia:
- Death of a loved one or ending of a significant relationship
- Divorce or breakup that leaves you living alone
- Moving away from family and friends
- Remote work or work-from-home arrangements (sudden increase in solitude)
- Empty nest syndrome when children leave home
- Pandemic-related isolation (lockdowns, social distancing)
- Retirement with loss of daily social contact
The COVID-19 pandemic, in particular, triggered or intensified autophobia for many people. Extended periods of isolation, combined with anxiety about health and safety, created a perfect storm for fear-of-being-alone symptoms to develop or worsen.
Genetic & Biological Factors
Research suggests some people may be genetically predisposed to anxiety disorders:
- Family history of phobias or anxiety disorders
- Gene variations that affect anxiety processing
- Amygdala hyperactivity (the brain’s fear center)
- Neurochemical imbalances affecting serotonin and other neurotransmitters
Studies show specific phobias were found to be higher in females compared to males and higher in higher-income countries compared to lower-income countries.[^3]
Important: Having one or more risk factors doesn’t mean you’ll definitely develop autophobia. These are simply factors that may increase susceptibility.
When to Seek Professional Help
It’s normal to prefer company over solitude, but autophobia crosses into territory that requires professional support. Consider reaching out to a mental health professional if:
- Your fear interferes with daily life (work, school, basic activities)
- You’re avoiding necessary activities because you’d have to do them alone
- Your relationships are suffering due to clinginess or dependency
- You’re experiencing panic attacks when alone or thinking about being alone
- You can’t sleep when you’re by yourself
- You’re using substances (alcohol, drugs) to cope with being alone
- You feel depressed or hopeless about your situation
- You’re having thoughts of self-harm or suicide
Crisis Resources (Available 24/7)
If you’re in crisis or experiencing thoughts of self-harm:
- SAMHSA National Helpline: 1-800-662-4357 (free, confidential, 24/7)
- Crisis Text Line: Text HOME to 741741
- National Suicide Prevention Lifeline: 988 or 1-800-273-8255
- Emergency: 911
You don’t have to handle this alone. These helplines connect you with trained professionals who understand what you’re going through.
Treatment Options That Actually Work
Here’s the good news: autophobia is highly treatable. With the right combination of therapy, strategies, and—when needed—medication, most people see significant improvement. Treatment success rates for specific phobias are among the highest for any mental health condition.
Cognitive Behavioral Therapy (CBT)
CBT is the gold standard for treating autophobia. This evidence-based therapy helps you identify and change the thought patterns fueling your fear.
How it works:
- Identify negative thoughts: “I’ll have a medical emergency and no one will help me”
- Challenge the beliefs: “What evidence do I have that this will happen? How likely is this really?”
- Replace with realistic thoughts: “I have my phone. I know how to call for help. Most people live alone safely.”
- Learn coping skills: Practical techniques to manage anxiety when it arises
What to expect: Weekly sessions lasting 12-20 weeks, with homework between sessions to practice new skills.
Exposure Therapy (ERP)
Exposure and Response Prevention therapy gradually helps you face your fear in a controlled, safe way.
The process:
- Create a fear hierarchy: Rank situations from least to most anxiety-provoking
- Start small: Perhaps being alone for 5 minutes with someone in the next room
- Gradually increase exposure: Extend time alone, increase distance from others
- Practice without safety behaviors: Eventually eliminate “crutches” like constant phone contact
- Repeat until anxiety decreases: Your brain learns that being alone isn’t actually dangerous
Example progression:
- Week 1-2: Alone in a room for 10 minutes (person in house)
- Week 3-4: Alone for 30 minutes (person in house)
- Week 5-6: Alone for 1 hour (no one home)
- Week 7-8: Alone for an afternoon
- Week 9+: Comfortable being alone for extended periods
Research shows exposure therapy is remarkably effective—many people see significant improvement within 8-12 weeks.
Medication Options
While therapy is the primary treatment, medication can help manage symptoms, especially during early treatment:
Beta-blockers (Propranolol, Atenolol):
- Block physical symptoms like rapid heartbeat
- Taken before anxiety-provoking situations
- Not addictive
- May help prevent fear memory formation during exposure therapy
SSRIs (Selective Serotonin Reuptake Inhibitors):
- Sertraline (Zoloft), Paroxetine (Paxil), Escitalopram (Lexapro)
- Help with overall anxiety levels
- Taken daily
- Can take 4-6 weeks to feel full effects
Benzodiazepines (Alprazolam/Xanax, Lorazepam/Ativan):
- Fast-acting anxiety relief
- Use with caution: Highly addictive, especially for those with substance use history
- Typically prescribed only for short-term, occasional use
- Not recommended as long-term solution
Important: Medication alone rarely “cures” autophobia. It works best when combined with therapy to address underlying thought patterns.
Other Therapeutic Approaches
EMDR (Eye Movement Desensitization and Reprocessing):
- Particularly helpful if autophobia stems from trauma
- Uses bilateral eye movements to process traumatic memories
Acceptance and Commitment Therapy (ACT):
- Focuses on accepting anxiety rather than fighting it
- Teaches mindfulness and values-based living
Group Therapy:
- Connect with others experiencing similar fears
- Practice social skills and receive peer support
- Reduces feelings of isolation about your condition
Mindfulness-Based Therapies:
- Meditation and breathing techniques
- Helps you stay present rather than catastrophizing about being alone
Finding the Right Therapist
Look for a mental health professional who:
- Specializes in anxiety disorders or specific phobias
- Has experience with CBT and exposure therapy
- Is licensed (psychologist, psychiatrist, LCSW, LPC)
- Makes you feel comfortable and understood
Where to find help:
- Psychology Today therapist directory: psychologytoday.com/us/therapists
- Your insurance provider’s directory
- ADAA therapist finder: adaa.org/finding-help
- Local mental health clinics or community centers
Immediate Coping Strategies: What to Do When You’re Alone Right Now
If you’re experiencing anxiety about being alone right now, these techniques can help you manage in the moment. These aren’t cures, but they can reduce your symptoms enough to get through the next hour or day.
Grounding Techniques (5-4-3-2-1 Method)
When panic starts, ground yourself in the present moment:
- 5 things you can see: Look around and name them out loud
- 4 things you can touch: Feel different textures (couch, table, clothing)
- 3 things you can hear: Listen for any sounds (traffic, refrigerator hum, birds)
- 2 things you can smell: Notice scents (coffee, soap, fresh air)
- 1 thing you can taste: Have a mint, drink water, or notice your mouth’s taste
This interrupts your panic response and reminds your brain you’re in the present, not in danger.
Breathing Exercises
Panic triggers rapid, shallow breathing. Counter it with:
Box Breathing:
- Inhale for 4 counts
- Hold for 4 counts
- Exhale for 4 counts
- Hold for 4 counts
- Repeat 4-5 times
4-7-8 Breathing:
- Inhale through nose for 4 counts
- Hold for 7 counts
- Exhale through mouth for 8 counts
- Repeat 3-4 times
Challenge Your Thoughts
Write down or say out loud:
- The fear: “Something terrible will happen because I’m alone”
- The evidence: “What proof do I have? Has this ever happened before?”
- The reality: “I’ve been alone before and been fine. I have my phone. I know what to do in an emergency.”
Stay Connected (But Set Boundaries)
Healthy connection:
- Text a friend: “Having a tough day, but managing”
- Schedule a phone call for later
- Join an online support community
Avoid:
- Constant texting demanding immediate responses
- Calling people repeatedly
- Creating emergencies just to get attention
Create a “Solo Survival Kit”
Prepare for times alone:
- Comfort items: Favorite blanket, stuffed animal, photos
- Distractions: Puzzles, coloring books, engaging TV shows
- Calming tools: Essential oils, stress ball, fidget toy
- Emergency plan: Written steps for if panic escalates (breathing exercises, emergency contacts)
- Inspirational notes: Reminders that you’ve done this before and survived
Structure Your Alone Time
Morning alone:
- Make a detailed schedule
- Breakfast + coffee ritual
- Exercise or stretch
- Productive activity (cleaning, project)
- Mid-morning check-in with friend (scheduled)
Afternoon alone:
- Lunch prep (engaging activity)
- Hobby or interest
- Brief walk outside
- Structured relaxation time
Evening alone:
- Dinner routine
- Entertainment (movie, book, game)
- Relaxation before bed
- Bedtime routine
Structure reduces anxiety because your brain knows what to expect.
Progressive Muscle Relaxation
Tense and release each muscle group:
- Clench fists for 5 seconds, release
- Tighten arms, release
- Scrunch shoulders to ears, release
- Continue through entire body
This releases physical tension and gives you something to focus on.
Use Background Sounds Wisely
It’s okay to use noise temporarily:
- Nature sounds or white noise
- Podcasts or audiobooks (not just “any noise”)
- Music playlists
- Videos of people talking (ASMR, vloggers)
Goal: Gradually reduce dependence on constant noise over time as you work with a therapist.
Living with Autophobia: Long-Term Management Strategies
Recovery isn’t instant, but with consistent effort, you can build a life where being alone doesn’t control you. Here’s how to manage autophobia long-term.
Build Independence Gradually
Start small and increase:
- Week 1: 15 minutes alone daily
- Week 2: 30 minutes alone
- Week 3: 1 hour alone
- Week 4: Half a day alone
- Month 2: Comfortable with an evening alone
- Month 3+: Weekend alone
Track your progress: Keep a journal noting how you felt and what helped.
Develop a Healthy Relationship with Solitude
Reframe “alone time” as “me time”:
- Activities you enjoy: hobbies, reading, creative projects
- Self-care: bath, skincare routine, stretching
- Personal growth: learning something new, journaling
- Rest: guilt-free napping or doing nothing
Goal: Associate being alone with pleasure, not fear.
Practice Self-Compassion
When you slip up (and you will):
- Don’t catastrophize: One difficult day doesn’t erase progress
- Acknowledge feelings: “This is hard right now, and that’s okay”
- Remind yourself: “I’m learning a new skill. It takes time.”
- Be patient: Recovery isn’t linear
Strengthen Your Support System
Build healthy relationships:
- Communicate your needs without being demanding
- Express appreciation when people support you
- Respect others’ boundaries and time
- Work on secure attachment patterns in therapy
Join support groups:
- Online communities for anxiety disorders
- Local mental health support groups
- Specific phobia support forums
Maintain Healthy Habits
Physical health supports mental health:
- Regular exercise: Reduces anxiety naturally (even 20 minutes daily helps)
- Consistent sleep: Go to bed and wake at same times
- Balanced nutrition: Avoid excess caffeine and sugar
- Limit alcohol: It worsens anxiety long-term
- Hydration: Dehydration can mimic anxiety symptoms
Continue Therapy Maintenance
Even after initial improvement:
- Check-ins with therapist (monthly or as needed)
- Booster sessions during stressful times
- Regular practice of CBT techniques
- Continued exposure practice
Plan for Setbacks
Identify high-risk situations:
- Major life changes (moving, breakup, job change)
- Increased stress levels
- Seasonal changes (winter isolation)
Have a relapse prevention plan:
- Warning signs to watch for
- Immediate strategies to implement
- When to call therapist
- Emergency contacts
Frequently Asked Questions About Autophobia
Is autophobia a mental illness?
Yes, autophobia is classified as a specific phobia, which is a type of anxiety disorder. While it’s not listed as a standalone disorder in the DSM-5, it falls under the category of “specific phobia—situational type” (code 300.29).[^1] It’s a legitimate mental health condition that requires treatment, not a character flaw or something you can simply “get over.”
Can autophobia be cured completely?
There’s no single “cure” that eliminates autophobia overnight, but it’s highly treatable. Most people who complete therapy (particularly CBT and exposure therapy) experience significant reduction in symptoms—many to the point where the phobia no longer interferes with their daily life. Think of it as managing rather than curing: you learn skills to control the fear instead of letting it control you. With consistent effort, many people reach a point where they’re comfortable being alone.
How do I stop panicking when I’m alone?
In the moment, try these steps:
- Name it: Say out loud “This is a panic attack. It will pass.”
- Use the 5-4-3-2-1 grounding technique (described above)
- Control your breathing: Use box breathing or 4-7-8 method
- Change your position: Stand up, stretch, walk to another room
- Focus on one task: Do dishes, organize a drawer, anything requiring attention
- Call your support person (if you’ve discussed this in advance)
- Remind yourself: “I’ve survived this before. I will survive it again.”
Long-term: Work with a therapist to address underlying fears and practice gradual exposure.
Is fear of being alone the same as separation anxiety?
They’re related but different. Separation anxiety disorder specifically involves excessive anxiety about being separated from specific attachment figures (usually parents in children, or romantic partners in adults). Autophobia is more general—it’s about the fear of being alone itself, not necessarily about separation from specific people. That said, they can overlap, and someone might experience both.
Can autophobia develop suddenly in adulthood?
Yes. While many phobias begin in childhood, autophobia can develop at any age. Common adult triggers include:
- Traumatic event while alone (home invasion, medical emergency)
- Death of a spouse or loved one
- Difficult divorce or breakup
- Major life transition (retirement, children leaving home)
- Development of another anxiety disorder
- Pandemic-related isolation
Even if you’ve been comfortable alone for years, a significant trigger can spark autophobia in adulthood.
How do I explain autophobia to family and friends?
Try this approach:
“I’m dealing with something called autophobia—it’s an anxiety disorder where I have intense fear and panic when I’m alone, even though I know I’m safe. It’s not about not liking my own company; my brain genuinely believes something bad will happen when I’m by myself. I’m working with a therapist on it, but I wanted you to understand so you know why I sometimes [specific behavior: ask you to stay on the phone, need reassurance, etc.]. I’m not being needy or dramatic—this is a real condition, and I’m actively working to get better.”
What to ask for:
- Patience as you work through this
- Understanding that some behaviors stem from the phobia
- Support without enabling (they shouldn’t rearrange their lives completely)
- Scheduled check-ins rather than on-demand availability
Does autophobia mean I have abandonment issues?
Not necessarily, but they often co-occur. Autophobia is specifically about fearing being alone, while abandonment issues involve fearing people will leave you. However:
- Many people with autophobia also fear abandonment
- Childhood abandonment can cause autophobia
- Both respond well to similar therapeutic approaches
- A therapist can help you sort out which is the primary issue
Research demonstrates a strong connection: fear of abandonment was positively correlated with both attachment insecurity (r = .62, p < .001) and psychosomatic symptoms (r = .51, p < .001).[^9]
What’s the difference between autophobia and codependency?
Autophobia is an anxiety disorder—a specific phobia of being alone. Codependency is a pattern of relating to others where you rely excessively on relationships for self-worth and identity. While autophobia can contribute to codependent behaviors (staying in unhealthy relationships, being excessively clingy), they’re not the same thing. You can have autophobia without being codependent, and vice versa. Often, though, treating autophobia also involves addressing any codependent patterns with a therapist.
Can medication alone treat autophobia?
No. While medication can help manage symptoms—especially in the short term—it doesn’t address the underlying thought patterns and fears driving autophobia. The most effective approach combines medication (if needed) with therapy. Think of medication as a tool that makes therapy more effective by reducing symptoms enough that you can engage in exposure exercises and CBT work. Some people use medication temporarily during early treatment, then taper off as they build coping skills.
How long does treatment take?
It varies by individual, but here are typical timelines:
- CBT: 12-20 weekly sessions for significant improvement
- Exposure therapy: 8-12 weeks of consistent practice
- Noticeable changes: Often within 4-6 weeks of starting therapy
- Long-term management: Ongoing practice of skills, with check-ins as needed
Some people improve faster; others need longer. Factors that affect timeline include:
- Severity of symptoms
- Presence of other mental health conditions
- Consistency with therapy homework
- Support system quality
- Trauma history requiring processing
Remember: Progress isn’t linear. You’ll have good weeks and tough weeks.
Taking the Next Step: Your Path Forward
If you’ve read this far, you’re already taking the first step toward recovery. You’re educating yourself, seeking understanding, and looking for solutions. That takes courage.
Here’s what to do next:
If you’re experiencing autophobia symptoms:
- Schedule an appointment with your doctor or a mental health professional
- Start a journal tracking your symptoms, triggers, and anxiety levels (this helps with diagnosis and treatment)
- Practice one coping technique today (try the 5-4-3-2-1 grounding exercise)
- Reach out to someone you trust and share what you’re going through
- Be patient with yourself as you begin this journey
If someone you love has autophobia:
- Educate yourself (you’re already doing this—thank you)
- Listen without judgment when they share their fears
- Offer support but avoid enabling avoidance behaviors
- Encourage professional help and offer to help them find a therapist
- Set healthy boundaries while remaining compassionate
- Celebrate their progress, no matter how small
Resources for Further Support
National Organizations:
- Anxiety and Depression Association of America (ADAA): www.adaa.org
- National Institute of Mental Health (NIMH): www.nimh.nih.gov
- Mental Health America: www.mhanational.org
- National Alliance on Mental Illness (NAMI): www.nami.org
- SAMHSA (Substance Abuse and Mental Health Services Administration): www.samhsa.gov
Crisis Support:
- SAMHSA National Helpline: 1-800-662-4357
- Crisis Text Line: Text HOME to 741741
- 988 Suicide & Crisis Lifeline: Call or text 988
Online Communities:
- ADAA Online Support Group
- r/Anxiety on Reddit
- 7 Cups of Tea (free emotional support chat)
- Anxiety Social Net
Related Articles from AllThePhobias:
- Nomophobia: Understanding Fear of Phone Separation
- Arachnophobia: Complete Guide to Overcoming Spider Fear
- Thalassophobia: Why Deep Water Triggers Fear
- Acrophobia: Understanding and Managing Fear of Heights
Final Thoughts: You’re Stronger Than Your Fear
Living with autophobia can feel isolating and overwhelming. The constant anxiety, the panic when you’re by yourself, the strain on relationships—it’s exhausting. But here’s the truth: you are not broken, you are not weak, and you are absolutely not alone in this struggle.
With an estimated 19 million Americans experiencing specific phobias each year,[^2] thousands of people share your exact fear. And thousands more have learned to manage it, overcome it, and reclaim their independence. You can be one of them.
The fear might feel permanent right now, but it’s not. With the right treatment, support, and consistent practice, you can reach a point where being alone is comfortable—maybe even enjoyable. Where you can spend an evening by yourself without panic. Where you can live independently without constant fear.
That future is possible. You deserve that future.
Start small. Reach out for help. Practice one coping technique today. Give yourself grace on the hard days and celebrate the tiny victories. Every minute you spend alone building your tolerance is a win. Every therapy session is progress. Every time you challenge a fearful thought, you’re rewiring your brain.
You’ve survived every difficult moment so far. You have that same strength within you to face this fear and come out the other side.
You are not your fear. You are capable of healing. And you don’t have to do it alone.
References & Citations
[^1]: American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
[^2]: National Institute of Mental Health. (2017). Specific Phobia. Retrieved from https://www.nimh.nih.gov/health/statistics/specific-phobia
[^3]: Eaton, W. W., Bienvenu, O. J., & Miloyan, B. (2018). Specific phobias. The Lancet Psychiatry, 5(8), 678-686. doi:10.1016/S2215-0366(18)30169-X
[^4]: Wardenaar, K. J., Lim, C. C. W., Al-Hamzawi, A. O., et al. (2017). The cross-national epidemiology of specific phobia in the World Mental Health Surveys. Psychological Medicine, 47(10), 1744-1760. doi:10.1017/S0033291717000174
[^5]: Samra, C. K., & Abdijadid, S. (2023). Specific Phobia. In StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK499923/
[^6]: Bowlby, J. (1973). Attachment and Loss: Vol. 2. Separation: Anxiety and Anger. New York: Basic Books.
[^7]: Mikulincer, M., & Shaver, P. R. (2007). Attachment in Adulthood: Structure, Dynamics, and Change. New York: Guilford Press.
[^8]: Brennan, K. A., Clark, C. L., & Shaver, P. R. (1998). Self-report measurement of adult attachment: An integrative overview. In J. A. Simpson & W. S. Rholes (Eds.), Attachment Theory and Close Relationships (pp. 46-76). New York: Guilford Press.
[^9]: Maroufizadeh, S., Ghaheri, A., Almasi-Hashiani, A., & Mohammadi, M. (2018). The relationship between maternal attachment dimensions and fear of childbirth in nulliparous women: A crossroad between mental health and midwifery. Journal of Psychosomatic Obstetrics & Gynecology, 39(3), 203-209. doi:10.1080/0167482X.2017.1349870
Additional Evidence-Based Resources:
- Anxiety and Depression Association of America (ADAA). Understanding Specific Phobias. Retrieved from https://adaa.org/understanding-anxiety/specific-phobias
- Mayo Clinic. (2023). Specific phobias – Symptoms and causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/specific-phobias/symptoms-causes/syc-20355156
- Cleveland Clinic. (2022). Specific Phobias. Retrieved from https://my.clevelandclinic.org/health/diseases/24454-specific-phobias
- Substance Abuse and Mental Health Services Administration (SAMHSA). National Helpline. Retrieved from https://www.samhsa.gov/find-help/national-helpline
If you or someone you know is in crisis, please reach out immediately:
- SAMHSA National Helpline: 1-800-662-4357 (24/7, free, confidential)
- Crisis Text Line: Text HOME to 741741
- 988 Suicide & Crisis Lifeline: Call or text 988
This article is for educational purposes and should not replace professional medical advice. If you’re experiencing symptoms of autophobia, please consult with a licensed mental health professional for proper diagnosis and treatment.
About AllThePhobias.com
AllThePhobias.com is dedicated to providing evidence-based, compassionate information about specific phobias and anxiety disorders. Our mission is to help people understand their fears, find effective treatment, and reclaim their lives. All content is researched and written with input from mental health professionals and peer-reviewed scientific literature.
Last Updated: October 2025